A new report from the Center for Improving Value in Health Care (CIVHC) finds the use of alternative payment models (APM) for primary care has increased in Colorado, while APM use for overall medical payments (not including pharmacy or dental) has declined across all payers. This is the first comprehensive analysis of alternative payment models across all payers in Colorado, designed to track progress away from traditional fee-for-service (FFS) payment models. Results show that while APMs for primary care are increasing, not as much progress is being made for payments across all medical services.
As health care costs continue to rise in Colorado, policymakers, providers, payers, and others across the state have worked to identify ways to shift away from the long-dominant fee-for-service (FFS) model. APMs offer providers payment structures that incentivize high quality, coordinated and cost-efficient care. With a focus on value of services over volume in the traditional FFS model, APMs can reduce health care spending and improve overall health and outcomes.
CIVHC first began collecting data on APMs from health insurance payers in 2019, as a result of changes to the Colorado All Payer Claims Database (CO APCD) Data Submission Guide rule that occurred in late 2018. In early 2019, the Investments in Primary Care legislation passed, and since then CIVHC has been providing the Primary Care Payment Reform Collaborative, led by the Colorado Division of Insurance, with an annual analysis related to primary care APMs to support the Collaborative.
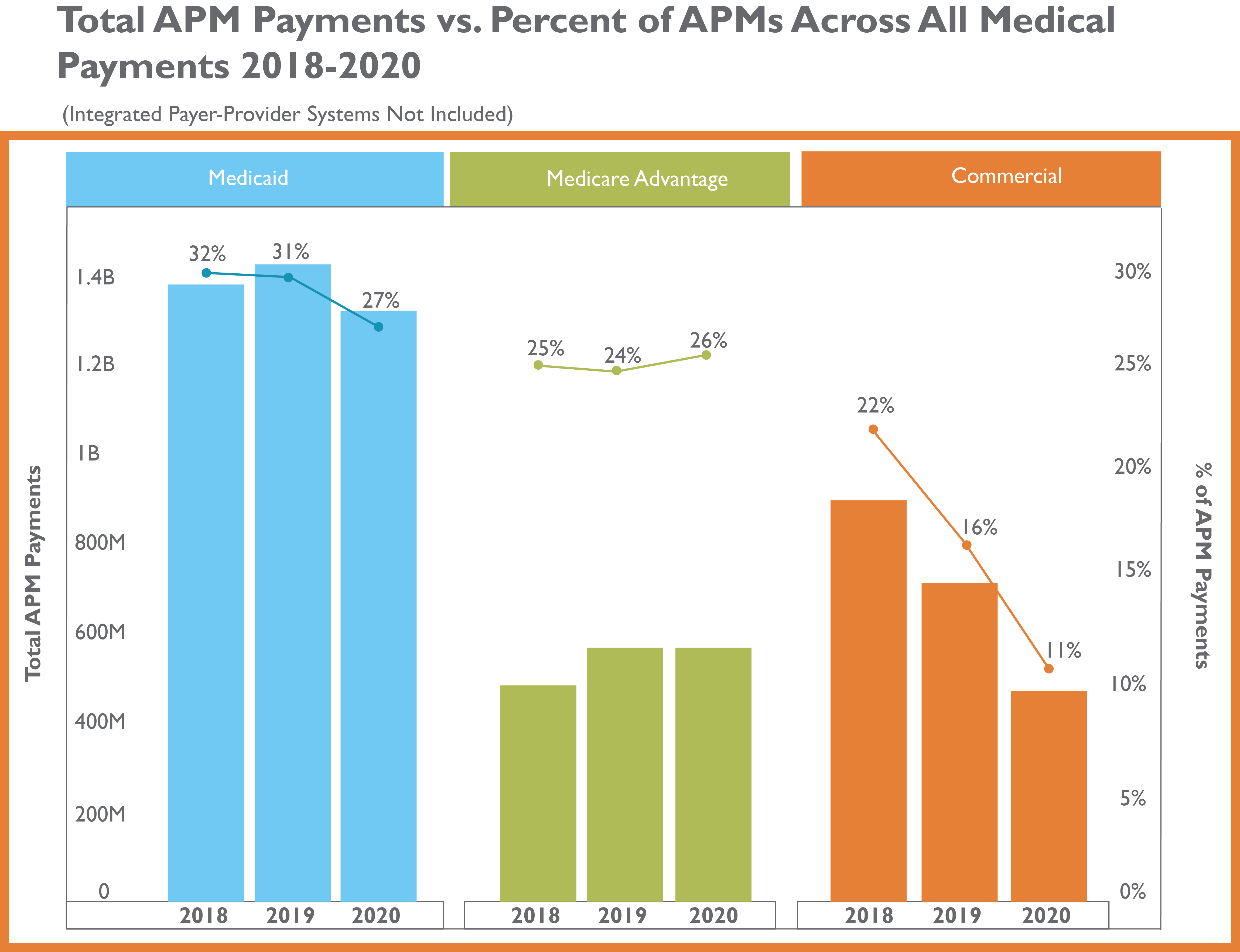
The data in this first public interactive report contains information on APM use across payers from 2018 to 2020, and provides not only primary care related APM information, but also APM data related to all medical spending in the state.
The analysis shows that, between 2018 to 2020, across all payers, value based[1] APM payments as a percent of all medical payments, excluding payments by payer-provider systems [2], dropped from 27% to 21%. However, value based APM payments as a percent of all primary care payments, excluding payments by payer-provider systems, remained at 21%.
All medical payments, excluding payments by payer-provider system:
Additional insights from the 2020 data in the analysis includes:
- For commercial payers, APMs accounted for 18% of all primary care payments.
- For all payers, the top Health Care Payment Learning & Action Network (LAN) Category was Pay for Performance, which accounted for 61% of APMs for all medical payments.
- For commercial payers, the top Health Care Payment Learning & Action Network (LAN) Category was APMS with Shared Savings, which accounted for 64% of APMs for all medical payments.
CIVHC’s ongoing collection and analysis of APM data give Colorado a way to track progress towards new payment models aimed at improving health and lowering costs. More insights, trend data, and information on the use of specific APM types can be found in the interactive report, part of CIVHC’s Affordability Dashboard.
For more information on the history of APMs, please review our APM issue brief, and for questions about the report or APM collection, please contact us at info@civhc.org.
[1] The Health Care Payment Learning & Action Network (LAN) Categories 3N and 4N are not linked to quality outcomes and therefore considered not value-based.
[2] Several Colorado payers are structured as integrated payer-provider systems and have a high portion of APM payments as compared to other commercial payers. These payers represent around a quarter of the commercially insured lives in Colorado.