Overview
During the 2022 Colorado legislative session, Senate Bill 22-068 was passed to increase health care payment transparency. The bill requests CIVHC, administrator of the Colorado All Payer Claims Database (CO APCD), to create a public report that displays payments made to Colorado health care providers for CPT (Current Procedural Terminology) codes and HCPCS (Healthcare Common Procedure Coding System) codes by county, Division of Insurance (DOI) Region, and statewide. The report includes the following:
- All current (effective in 2021) CPT codes and HCPCS with sufficient volume (statewide claim volume of 30 or more) for 2018-2023.
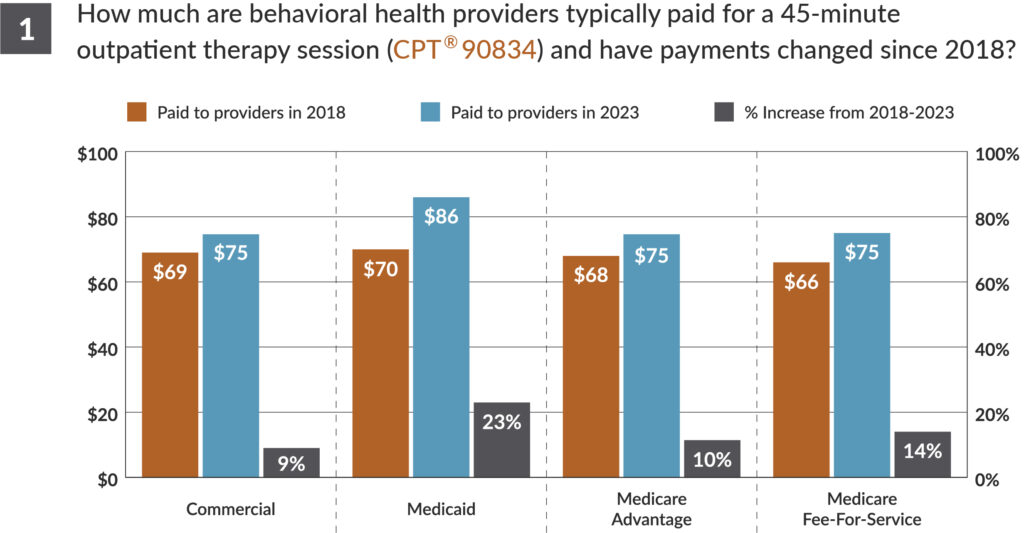
- Payer breakouts for Commercial, Medicaid, Medicare Advantage, and Medicare Fee-for-Service.
- Total allowed amounts (payer and patient payments combined) at the 25th, 50th, 60th, and 75th percentile, and average total allowed amounts.
- Anesthesiology payment calculations (see below for details).
View Senate Bill 22-068 for more information.
Use Cases
Self-Insured and Full Insured Employers
- Self-insured: Understand what you are paying for services verses other payers in your area and statewide. Use this information to discuss rates with your insurance broker or TPA/ASO.
- Fully-insured: Point employees to the tool if they have questions about how much a service may cost, or related to provider bills they received and whether the price was reasonable.
Health Insurance Payers and Health Care Providers
- Benchmark how your payments for services compare to your peers. Use this information when discussing annual rate changes.
State Agencies and Policy Makers
- Identify variations in payments for procedures across the state. Determine where there may be opportunities to reduce price variation and increase access to care.
Consumers and Advocacy Organizations:
- Use the tool to understand common prices for specific services, and talk to your providers and/or health insurance payer if there is a discrepancy in prices for services you plan to receive or did receive.
Learn More
Key Considerations:
- The analysis includes all public and private health insurance payers submitting data to the Colorado All Payer Claims Database (CO APCD), which represents the majority of covered lives (70% of medically insured) in the state. The CO APCD does not include roughly half of the self-insured employer covered lives and does not include federal programs such as Tricare, Indian Health Services and the VA.
- This analysis is based on fee-for-service payments only and does not include supplemental payments, capitated payments or payments made through Alternative Payment Models (APMs).
- The data only includes payments for in-network providers for commercial, Medicaid and Medicare Advantage claims. Medicare FFS data in the CO APCD does not indicate in- vs. out-of-network providers, and therefore may include some out-of-network payments.
- Payments represent total allowed amounts (plan and patient paid) for the professional/provider portion of the claim only. Payments do not include any facility fees or other payments that may have been billed for the service.
- Codes with average payments that are greater than or less than the percentile payments are driven by a small number of high or low cost claims.