PROFILE: Advancing Care Together Program
 Behavioral health includes mental health and substance abuse, as well as life stressors and crises or stress-related physical symptoms. Over half the people with a behavioral health disorder do not receive treatment for their condition. Yet, 80 percent of those with a behavioral health disorder do see a primary care provider at least once a year. The divorce of mental and physical health into separate avenues of treatment is long-standing, yet providers today are questioning the wisdom of the split. Through the Advancing Care Together (ACT) program, the department of family medicine at the University of Colorado School of Medicine reunited these two arenas of health care.
Behavioral health includes mental health and substance abuse, as well as life stressors and crises or stress-related physical symptoms. Over half the people with a behavioral health disorder do not receive treatment for their condition. Yet, 80 percent of those with a behavioral health disorder do see a primary care provider at least once a year. The divorce of mental and physical health into separate avenues of treatment is long-standing, yet providers today are questioning the wisdom of the split. Through the Advancing Care Together (ACT) program, the department of family medicine at the University of Colorado School of Medicine reunited these two arenas of health care.
ACT, a five year initiative funded by the Colorado Health Foundation, integrated physical and behavioral health at 11 facilities in Colorado. Each facility received nominal funding for implementation ($150,000 over three years) with the intent that the innovations would be sustainable once the grant period ended. Practices applied to participate and a steering committee chose those that represented a spectrum of business models and populations served, as well as a diversity of ideas. It was important that the facilities’ situations and business models be different to identify potential challenges in implementation, but common enough to allow for similar organizations to benefit from lessons learned.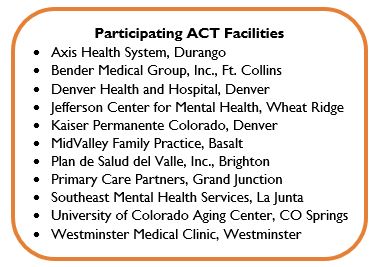
Nine primary care and two behavioral health practices joined the initiative. “The separation of treatment for people with both emotional and behavioral problems into physical and mental compartments, and two systems of care, was a mistake,” explains Dr. Larry Green, former director of ACT
While no two participating ACT facilities are alike, all faced similar challenges during the implementation phase of the program. “Progress on actually changing clinical practice to integrate care has been slow, not so much because of neglect, but because it is hard, often challenged by history, clashing cultures, and institutional barriers.”
Identifying and integrating new staff members was a particular hurdle for all participants. Successfully adding a behavioral health provider to a physical health practice (and vice versa) requires balance within the organization and a like-minded team. Often, office workflow structures favor one discipline or the other, resulting in disproportionate care across physical and behavioral health. Culture clash between provider types using different approaches and processes also made assimilation difficult.
Technology also proved to be a stumbling block for practice transformation as existing electronic health record (EHR) platforms are not designed to collect both behavioral and physical health data. Compounding the challenge, behavioral health data gleaned from patient surveys could not always be easily aggregated and analyzed.
Additionally, reimbursement and billing presented significant concerns. Combined behavioral health and physical care visits, or simply an appointment with each in one day, often fall outside current limitations set by insurance companies.
Green describes the root of these challenges as evolution moving too fast for the existing system. “Innovation often outpaces the speed at which health policy changes to accommodate the innovation. We have to acknowledge that one size doesn’t fit all.”
In spite of multiple challenges, the successes of the initiative were undeniable. Across the practices, significant care coordination improvements were made including:
- Teams working together to facilitate better care for patients (provide for warm handoffs, coordinated consultations, etc.);
- Both types of clinicians integrated into care teams;
- Building or repurposing of available space to allow for real time consultations and hand-offs;
- More universal screening of patients; and
- Collected data that supports the case for integrated care and needed policy change.
ACT was also able to move the needle on payment reform and reimbursement as a result of its success. In November, University Physicians, Inc, (UPI) and the University of Colorado Hospital (UCH) implemented a new contracting and reimbursement strategy to support integrated care.
There is no doubt that policy changes, delivery system redesign, and payment reform are significant and impressive achievements; however, the human side of ACT truly drives home the benefits of the program as illustrated by Patrick’s story.
Patrick, an entrepreneur and aspiring competitive athlete in Basalt, injured himself while playing tennis – an injury so severe, it resulted in partial paralysis. Adjustment to his new life and limitations did not come easy for Patrick and he fell into alcohol abuse and depression. His primary care provider helped him back onto the road to recovery by setting aside time to speak to Patrick about his condition and activities at each appointment and suggesting behavioral health intervention as his condition seemed to deteriorate. With his primary care physician working alongside his counselor, Patrick benefited from the support necessary to heal, both physically and mentally.
Stories like Patrick’s are not uncommon across the practices and it is these successes that keep them committed to the whole patient, both body and mind. “Though integration is hard, these practices are not returning to their former states,” confirms Green, “for them, integrated, comprehensive care is here to stay. They continue to share their struggles and breakthroughs with each other, and we in the CU Department of Family Medicine, continue to share resources with them to help with this journey.”
Integrated care is gaining more traction in Colorado and nationally as funders, payers, providers and others are realizing the benefit to patients, families and the health care system. As one example, Colorado received federal funding in late 2014 for the State Innovation Model that aims to advance integrated health across multiple provider groups in the state.
Read more about ACT successes and lessons learned in a special issue of the Journal of the American Board of Family Medicine, or visit the ACT website.
Previously published as part of CIVHC’s Spotlight on Innovation series.

