As administrator of the Colorado All Payer Claims Database (CO APCD), CIVHC is required by statute to maintain the database and continually improve the quality and utility of the data. One of the most important ways CIVHC makes the data better and more useful is by updating the CO APCD Rule and Data Submission Guide (DSG) each year. This is done in collaboration with the Department of Health Care Policy and Financing (HCPF), Division of Insurance (DOI), and health insurance payers across the state.
CIVHC follows the HCPF Executive Rule Change Process to propose new data submission requirements and updates. This is how new data elements are added, clarified, or eliminated, and the CO APCD Rule (Colorado Regulation 1.200) gets updated accordingly. Each update CIVHC proposes is to ensure the data is as robust, comprehensive, accurate and usable as possible and provides the most benefit to Colorado. Generally, these updates include:
- Standardization or clarification of elements already being collected, and/or
- Addition of new elements that will further align CO APCD data submissions with the Common Data Layout (CDL) being used by APCDs throughout the nation
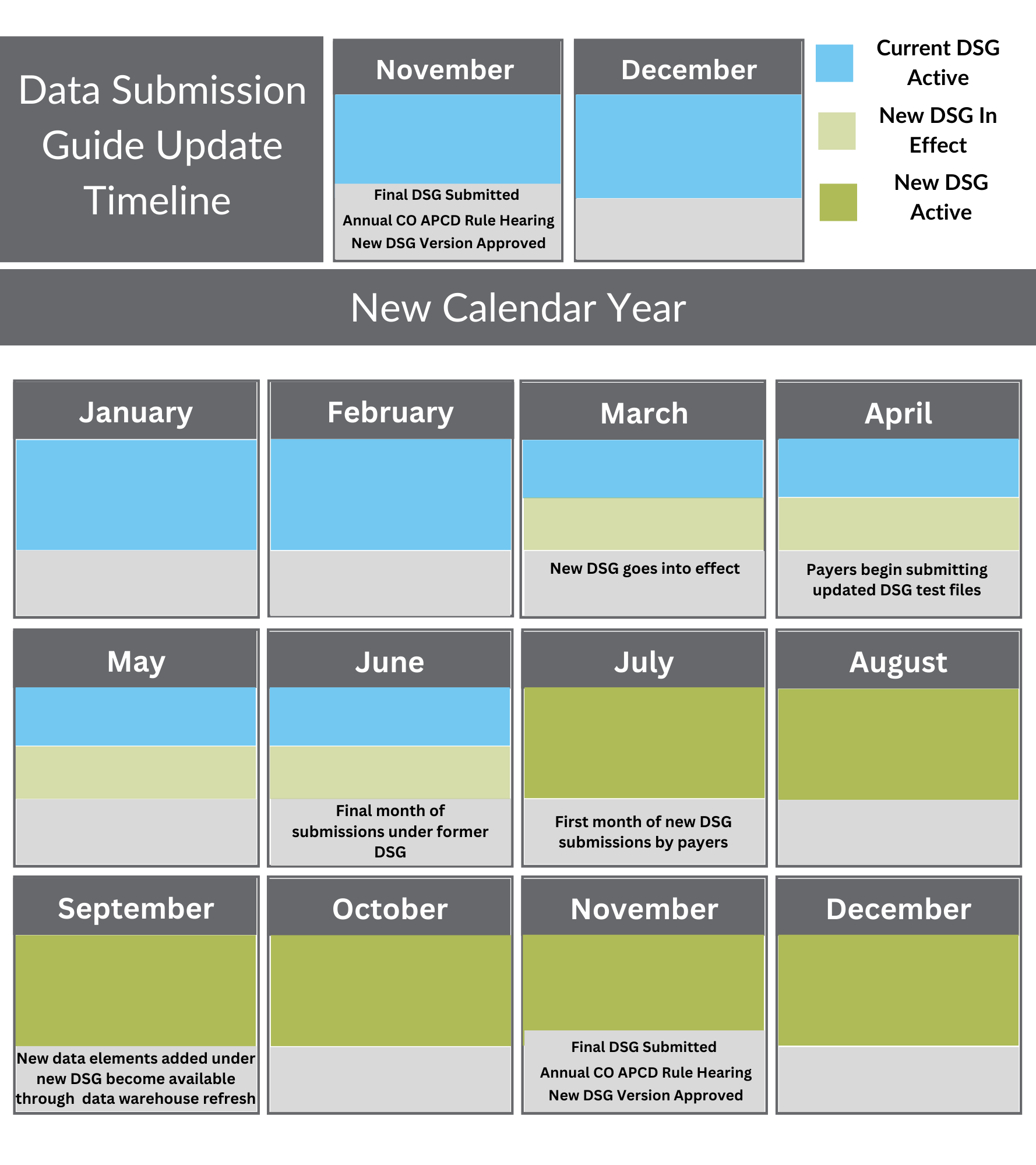
Each DSG update and Rule Change cycle takes place over a year. The CIVHC team starts looking toward changes to the next DSG early in the year, immediately after approval of changes proposed for the previous update. Throughout the summer and fall, CIVHC hosts several calls with payers to describe the proposed changes, answer questions, and receive feedback. After multiple drafts, payer feedback calls, comment periods, and virtual public review meetings, CIVHC and HCPF present the final proposed changes in a rule change hearing that typically takes place in November.
The new DSG and the revised CO APCD Rule typically take effect in March of each year. The previous DSG remains active through June, with payers having a 120-day grace period from the effective date to prepare their systems and submit test files before formal submission of files later in the year. Payers’ first submission of files under the new DSG is required in July 2025.
DSG 16 Updates
DSG 16 was the latest to be approved and introduced several notable updates to file collection, including the introduction of a new Annual File to collect information on capitation payments. CIVHC collaborated with payers throughout the last year to integrate these reporting enhancements into their systems, and the process is still ongoing to ensure timely, accurate submission of these files.
Additional updates to the DSG under version 16 primarily focus on enhancing data validation and improving the granularity of submitted data. The most significant addition is the inclusion of new medical, pharmacy, dental, and vision Per Member Per Month (PMPM) fields across all file types. These fields will assist with data validation and allow CIVHC to compare PMPM amounts calculated by payers against what is actually submitted to the CO APCD to ensure the data aligns with expectations.
Further notable updates to DSG 16 to improve submission quality are outlined by file type below.
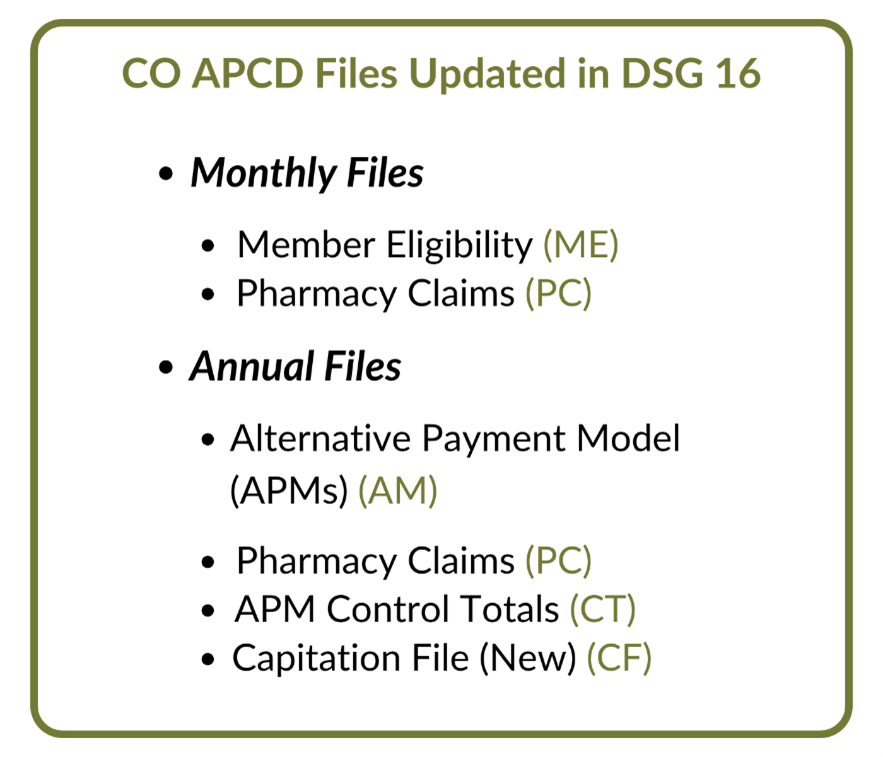 Monthly Files: Membership Eligibility (ME) & Pharmacy (PC) Updates
Monthly Files: Membership Eligibility (ME) & Pharmacy (PC) Updates
The most significant updates to the Membership Eligibility files are:
- Discontinuation of Vision and Dental Product Insurance Type Codes – DSG 16 removes these codes and submitters must now use more accurate codes which separate eligibility information and claim details. A member’s dental and vision coverage are tracked in dedicated Membership Eligibility file fields while actual claims are tracked through medical claims files to improve clarity and accuracy.
- Addition of a Colorado PBM Registration Number in Pharmacy Claim Files – This field was added to capture the Colorado Pharmacy Benefit Manager (PBM) Registration Number following a Department of Insurance (DOI) requirement for PBMs to register by June 2024. This will help distinguish PBMs within the data.
- Addition of a Formulary Tier Number in Pharmacy Claim Files – The Formulary Tier Number indicates the cost-sharing level of a drug in a health plan’s formulary, which identifies how much a patient will pay for a medication based on its tier. This will improve analysis of drug pricing and patient cost-sharing.
- Addition of Benefit Plan Code and Description in Pharmacy and Medical Claim Files – Specific identifiers are now required that identifies a member’s benefit plan and coverage type. These fields will be determined and submitted only by Colorado’s Medicaid program, managed by HCPF.
Annual File Updates
Updates to Annual Files focus primarily on introducing elements to improve data granularity and capture more detailed provider and payer information, most notable with the adoption of the NAHDO Non-Claims Payment reporting layout. New fields were added to the Alternative Payment Model and APM Control files to capture member count, member responsibility amount, and amount paid for behavioral health services.
Additionally, DSG 16 introduces a new file type – a Member Capitation File – designed to capture details about capitated payment arrangements between payers and providers. Capitation is a payment model where providers are paid a set amount for a patient regardless of the services the patient uses or number of visits. This new file allows CIVHC to collect data on these arrangements to provide transparency on APM models and better understand care and delivery structures.
CO APCD Rule
Updates to the CO APCD Rule were minimal and involved updating dates and titles to fall into alignment with DSG 16.
As payers work to prepare for changes under the latest DSG, CIVHC is already working to develop the next DSG update in anticipation of what elements, insights, and data collection enhancements will ensure the CO APCD continues to be a vital resource to improve health care and lower costs for Coloradans.
If you have questions regarding any DSG changes or would like more information on completeness and availability of data, please contact info@civhc.org.
