There is a staggering array of information in the Colorado All Payer Claims Database (CO APCD). So much information that it can be difficult to keep track of the different types and their various combinations, much less their infinite applications. The CO APCD Insights Dashboard shows us that, as of June 2022, there were more than 870 million claims in the database, representing nearly 70% of covered lives in Colorado. But what type of information is collected in all those claims?
You may be familiar with the foundational claim types that are submitted to the CO APCD: medical, pharmacy, and dental. But what do each of those claim types tell us about a patient’s specific service or procedure? A fuller understanding of what information is collected in these claims can help inform on the versatility of options available when using CO APCD data to improve care, lower costs, and make Colorado healthier.
Let’s take a look through all the claim types and the kind of information that is typically provided in each one. Now, different types of facilities and providers do use different versions of these forms, so we will be giving a general overview of the types of information collected in each claim type rather than going through a bunch of complicated (and boring) forms.
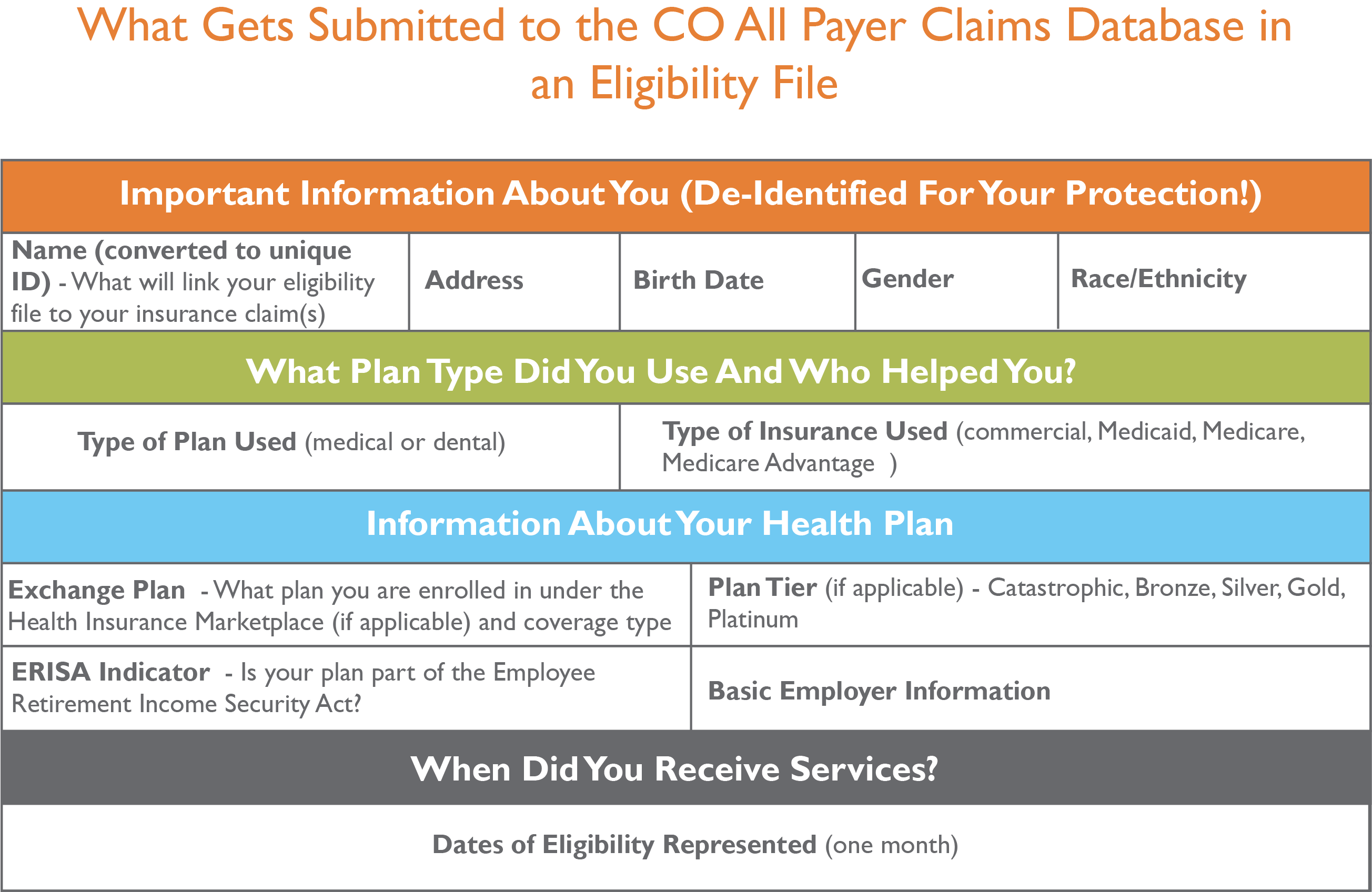
Basic Information Collected in Eligibility Files
No, eligibility files are not claims. But we are starting with them because collecting eligibility files in the CO APCD tells us who in Colorado’s insured population is using their insurance, and who isn’t. This allows us to report on utilization of insurance with tools like CIVHC’s Community Dashboard, which tracks health care utilization among healthy individuals and insurance non-users.
Basically, eligibility files tell us who used their insurance within a reporting period (the reporting period for eligibility files is one month) and how much. From there, the files are connected to the claims explained below to give further information about the types of services received, providers, costs, and other details. Insurers submit both eligibility files and claims with the same (de-identified) Member ID, allowing them to be linked and helping CIVHC to further verify claims collected from insurers.
Medical, Professional, Dental, and Pharmacy Claims
Claims for services or prescriptions include basic information about why you saw a provider, who you visited, and what happened while you were there – all information which forms the basis for the facility (hospital or provider group) part of the cost of the visit. The breakouts below focus on what is collected in the CO APCD.
Basic Information Collected in Medical Claims
Claim Dissection Table - Medical ClaimBasic Information Collected in a Professional Claim
Professional Claim Dissection Table_2020Basic Information Collected in a Dental Claim
Dental Claim Dissection Table 2020Basic Information Collected in a Pharmacy Claim
Pharmacy Claims Chart
