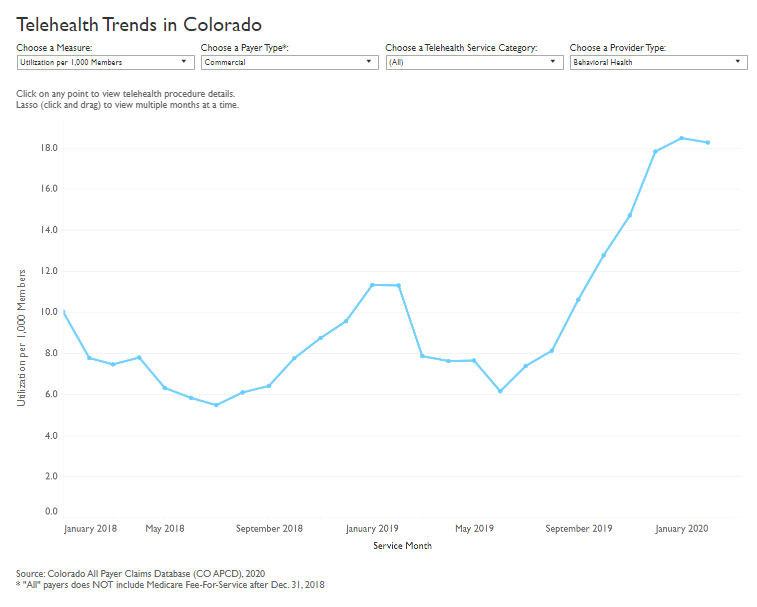
A new analysis using data from the Colorado All Payer Claims Database (CO APCD) shows use of telehealth services in Colorado was on the rise before the onset of the novel coronavirus pandemic. From January 2018 to February 2020, telehealth utilization per 1,000 members increased from 57 to 75.9 (33%) for commercial, 28.9 to 55.1 (91%) for Medicaid, and 125.7 to 142 (13%) for Medicare Advantage members. In January 2020 alone, there were 19,000 telehealth visits in Colorado.
The results, produced by Center for Improving Value in Health Care (CIVHC), serve as a benchmark to understand telehealth services prior to the onset of COVID-19 and will be updated regularly to help stakeholders evaluate changes in the health care system as a result of telehealth use before, during and after the pandemic.
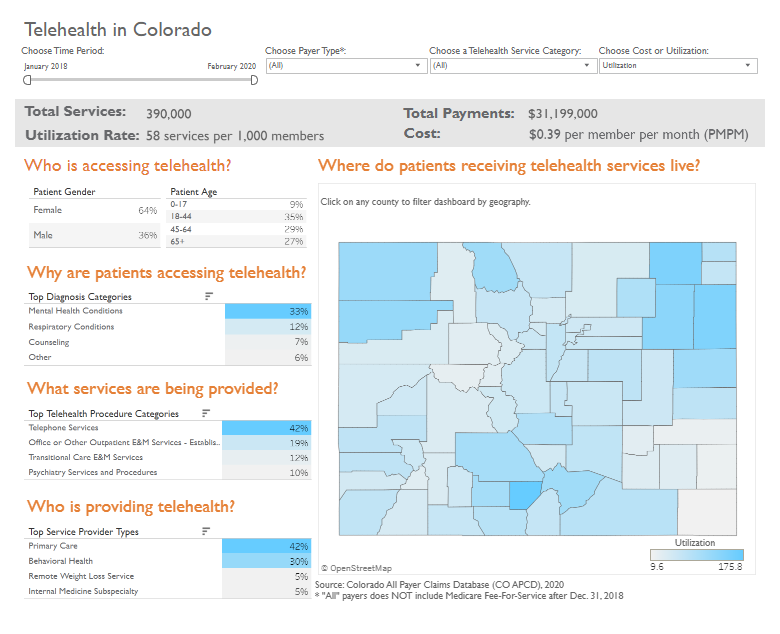
Users of the interactive reports can view how telehealth use and cost differ by health insurance payer type (Medicaid, Commercial, Medicare Advantage, Medicare fee-for-service), and type of telehealth service. For the state as a whole or by selecting each county, users can see telehealth use by age and gender, diagnosis, and provider type to answer a number of important questions including:
- What types of telehealth services are being provided?
- Why are patients using telehealth services?
- What types of providers deliver the most telehealth services?
- How does use of telehealth differ between counties across the state?
- Has utilization of telehealth changed over time?
- How much do we spend on telehealth per person and as a state?
Results show that between January 2018 and February 2020, over 390,000 telehealth services were provided to Coloradans resulting in over $31 million in payments to providers. Females use telehealth services more often than males (64% compared to 36%), and young adults aged 18-44 use telehealth services more than other age groups.
The most frequent reason telehealth was used was to treat mental health conditions (33%) followed by respiratory conditions (12%) and counseling (7%). Primary care providers have historically provided the most telehealth, followed by behavioral health providers. Telephone services are the most commonly provided telehealth offering followed by established patient office visits and transitions of care services offered remotely. It is important to note when viewing the report that telephone services for established patients were reimbursed by commercial and Medicare Advantage plans prior to 2020, but were not reimbursed by Medicare Fee-for-service and Medicaid until April and March 2020, respectively.
Several rural counties have higher per person telehealth utilization rates compared to their urban counterparts. Alamosa county leads the state with the highest overall telehealth utilization rates, 93% of which were for mental health conditions. Some rural counties, however, have very low telehealth rates which may reflect a number of barriers including insufficient access to broadband services and technology.
Using telehealth services to access behavioral health providers is on the rise. Between January 2018 and February 2020, commercially insured patients increased their use of telehealth with behavioral health providers the most (83%), followed by Medicaid patients (56%) and Medicare Advantage patients (15%).
CIVHC plans to update the telehealth analysis frequently to enable evaluation of the impact of the COVID-19 pandemic on use of telehealth services and patient outcomes long-term.
- View the interactive report
- Read more on telehealth in Colorado from the Colorado Health Institute
- More COVID-19 related analyses from CIVHC: