PROFILE: Assessing Health Systems Across the Nation
![]() Click the player above to listen to CIVHC’s VP of Research and Innovation, Kristin Paulson, JD MPH, chat with the Commonwealth Fund’s Senior Research Director, Douglas McCarthy. Access the presentation slides here.
Click the player above to listen to CIVHC’s VP of Research and Innovation, Kristin Paulson, JD MPH, chat with the Commonwealth Fund’s Senior Research Director, Douglas McCarthy. Access the presentation slides here.
 The Commonwealth Fund is a nonpartisan research foundation established in 1918 with the broad charge to enhance the common good. It is committed to ensuring that everyone in the U.S., regardless of their income or health, can get the health care they need and that the care they receive is the best and most efficient it can be.
The Commonwealth Fund is a nonpartisan research foundation established in 1918 with the broad charge to enhance the common good. It is committed to ensuring that everyone in the U.S., regardless of their income or health, can get the health care they need and that the care they receive is the best and most efficient it can be.
Project Summary: Since 2006, The Commonwealth Fund has produced 12 health system scorecards examining performance at the national, state, and local level. They have also conducted case studies examining more than 10 0 promising practices for improving health care.
0 promising practices for improving health care.
The scorecards rank states and local areas on more than 40 indicators of health care access, quality, cost, and outcomes. They reveal wide geographic variations in performance as well as racial and income-related disparities in care both within and between states. Case studies dig deeper into such findings to explore promising practices for delivering better, more efficient health care.
The Commonwealth Fund uses publicly available data from federal agencies such as the U.S. Census Bureau, the Centers for Disease Control and Prevention, and the Centers for Medicare and Medicaid Services to generate the Scorecards. Findings are widely reported by the news media and serve as a catalyst to build awareness of gaps in performance and readiness for change when used by policymakers and stakeholder groups to reflect on ways in which policy and action can make a difference.
Benefit to Colorado: The Scorecards can provide valuable insight into how to improve health systems on a state-level. The recent case study of Pueblo, Colorado—one of 14 communities across the country that improved the most on the 2016 Local Scorecard—found that socioeconomic challenges and geographic isolation have fostered a sense of interdependence among local health care providers, who have leveraged the state’s Medicaid expansion to enhance access to care while improving coordination. Collaborative efforts such as the Pueblo Triple Aim Corporation build on state policy and use philanthropic dollars to accomplish local priorities while appealing to community pride.
A comparison of high- and low-performing states identified market, political, and cultural characteristics that can help or hinder health system improvement. Higher-performing states are more likely to have a history of continuous reform and government leadership; a culture of collaboration among stakeholders; transparency of price and quality information; and a congruent set of policies that focus on system improvement.
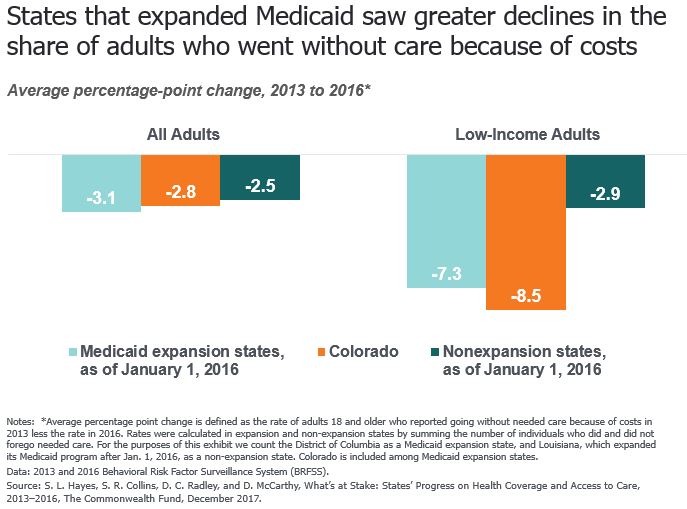
The 2017 State Scorecard found that states such as Colorado that accepted federal funding to expand their Medicaid programs under the Affordable Care Act (ACA) generally outperformed states that did not expand Medicaid. Colorado was one of five states that rose the most in the rankings, from 11th place in the 2013 baseline period, prior to the ACA’s major coverage expansions, to 6th place (tied with Iowa) in the 2015 post-expansion period.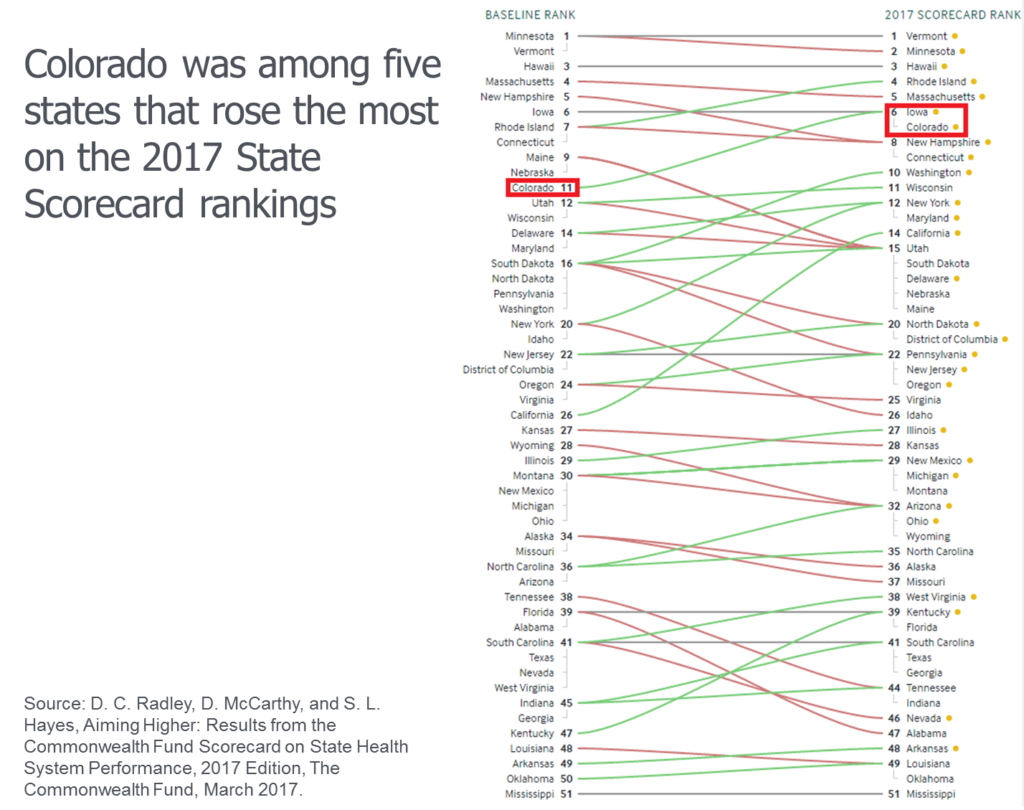 An update to the Scorecard’s Access Dimension, released in December 2017, found that Medicaid-expansion states such as Colorado saw greater reductions, on average, in the percentage of adults who reported they went without care because of its cost—especially among low-income adults. In Colorado, this rate fell from 15% to 12% among all adults (ages 18 and older) and from 29% to 21% among low-income adults (those with household income under 200% of the federal poverty level) between 2013 and 2016.
An update to the Scorecard’s Access Dimension, released in December 2017, found that Medicaid-expansion states such as Colorado saw greater reductions, on average, in the percentage of adults who reported they went without care because of its cost—especially among low-income adults. In Colorado, this rate fell from 15% to 12% among all adults (ages 18 and older) and from 29% to 21% among low-income adults (those with household income under 200% of the federal poverty level) between 2013 and 2016.
Visitors to the Commonwealth Fund’s Health System Data Center can view and download comparative state and local health system performance information; model the impact of improvements in each state’s performance through the Best State Interactive; and use the Quality–Spending Interactive to understand the “value relationship” between health care quality and spending in all regions of the country.