Evaluating Health Disparities Among American Indian and Alaskan Native Populations in Colorado
Profile
Denver Indian Center Inc. (DICI) is a vital urban cultural hub and community resource center for American Indians in Colorado. For over 50 years, it has empowered American Indian individuals and communities by promoting self-determination and mental, physical, and economic health through cultural enrichment, advocacy, and education.
Summary
DICI has partnered with National Jewish Health, a leading integrative medical center, to develop a culturally tailored provider education initiative. This initiative aims to train health care providers in culturally competent care, using a program that is data-driven and addresses the unique health challenges and social determinants of health (SDOH) that disproprotionately impact American Indian and Alaskan Native (AI/AN) communities. To support this initiative, the Center for Improving Value in Health Care (CIVHC) conducted an evaluation of AI/AN health disparities in Colorado using data from the Colorado All Payer Claims Database (CO APCD). This evaluation assesses the most frequently treated diseases among eligible AI/AN individuals compared to Non-Hispanic White (NHW) populations, their health care utilization patterns, including emergency department visits, hospitalizations, follow-up care rates and cost, and the role of SDOH—such as housing, employment, and income stability—captured through ICD-10 Social Needs Z-codes and American Community Survey (ACS) data. By contextualizing claims-based health care utilization data with ACS socioeconomic indicators, this study provides a comprehensive view of AI/AN health disparities in Colorado.
Findings
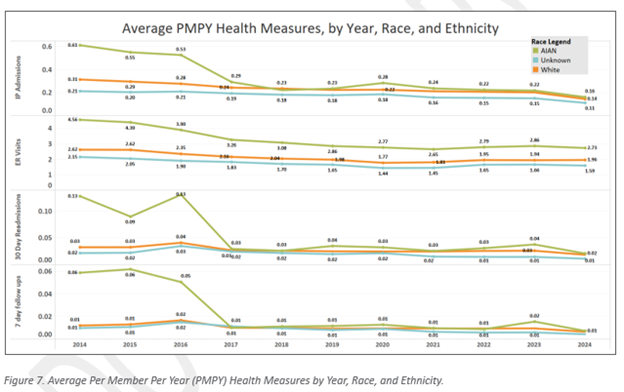
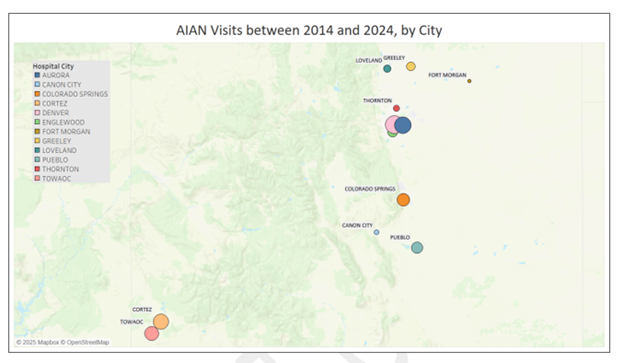
CIVHC’s evaluation describes the total eligible population included in the analysis, including eligibility trends, racial/ethnic distribution, age grouping, gender/sex representation, and insurance type. The findings provide foundational context for interpreting disparities in health care utilization, outcomes, and SDOH. The findings indicate that from 2014-2017, AI/AN populations exhibited higher inpatient admission rates and emergency department (ED) utilization, faced higher health care costs across all insurance types, and higher levels of disparity among all categories of social determinants of health compared to NHW individuals. Between 2018 and 2024, inpatient and ED utilization declined for AI/AN and NHW populations, but disparities remained. Also during this time, AI/AN populations continued to experience rising health care costs, particularly for those with commercial insurance and Medicare fee-for-service. Among AI/AN populations, metabolic and endocrine disorders were among the top five diagnosed conditions from 2014-2017, and though this number declined in the following years, they still remained among the top five diagnoses. Between 2018 and 2024, social determinants of health disparities between AI/AN and NHW populations widened. AI/AN individuals continued to experience higher levels of housing insecurity, economic instability, and lower access to health care compared to NHW individuals. The changes observed in 2018-2024 may be in part to the better identification of the AI/AN community in those years.
Benefit to Colorado
CIVHC’s evaluation services for DICI helps to ensure that the curriculum used in their educational programing is evidence-based and data-driven, enhancing its credibility and effectiveness in promoting health equity. These findings will support targeted policy recommendations, inform culturally responsive provider training, and guide strategic interventions to improve AI/AN health care access and outcomes in Colorado.