Each month, health insurance payers submit millions of medical, professional, pharmacy, dental, and vision claims for inclusion in the Colorado All Payer Claims Database (CO APCD). CIVHC continuously works closely with submitters to ensure they understand the submission requirements and that the process is as smooth as possible.
After submissions pass the initial validation tests and payers have been notified of acceptance, all data submissions pass into more extensive quality checks designed to make sure the data is accurate and credible.
Analysts compare the newly submitted data to over 100 submission benchmarks and look to ensure things like monthly payments per member, eligibility, total allowed amounts, and other measures compare reasonably with past submissions. These quality checks allow analysts to see if there are any unexpected anomalies that may result from data submission errors. Once all validation and quality assurance concerns have been addressed, the claims are processed and move into the CO APCD data warehouse.
Refreshing the Data Warehouse
While payers submit claims for processing each month, the data in the CO APCD is refreshed
and processed every other month.* The refresh process not only incorporates the two most recent months of claims but also reprocesses the entire CO APCD to continually improve the quality of the data. Reprocessing the entire database is important because it adds in historic claims that weren’t paid during the last submission cycle and can include resubmissions to correct identified data quality concerns, and claims that were revised since the initial adjudication process. In essence, the bi-monthly refreshes create a wholly new, updated, and improved CO APCD every time.
It is worth keeping in mind that while refreshes ensure that the CO APCD is continually being enhanced, it also means that data sets and analytics based on the database will not be 100% replicable in the future. Each output of the CO APCD during a specific two-month refresh span incorporates different data than the next, and it is possible that a data set or analysis with the same data elements and methodology in the future may show slightly varied results.
Ensuring Data Quality
Collaborative efforts between health insurance payers and the CIVHC intake team do not end after payers’ monthly submissions are ingested into the data warehouse. CIVHC analysts continue to work closely with payers to review each submission and identify opportunities to improve the quality of submitted data.
In 2022, CIVHC introduced the Submitter Quality Index (SQI), a measurement tool designed by CIVHC analysts to help assess the quality of data submitted to the CO APCD by health insurance payers. The SQI also gives an assessment of the overall health of data submitted to the CO APCD and allows CIVHC to track continued progress to enhance the quality of the entire database.
Implementation of the SQI is a fundamental step in CIVHC’s overall plan to continually improve data quality. While we use “data quality” as a catch-all term, it actually encompasses several different components under CIVHC’s definition.
The SQI assigns a numerical score to data submitted by payers, assessing over 25 common data fields for each type of file submitted (Eligibility Files, Medical Claims, and Pharmacy Claims), for a total of over 75 total common data elements. In each field, analysts check the accuracy and completeness of the submission, looking for errors such as an invalid field or one left blank.
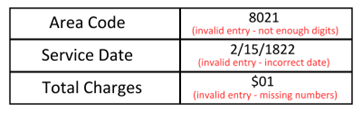
When all fields have been evaluated and scored, data fields receive a score from 0 (lowest) to 5 (highest possible), which evaluates the completeness and accuracy of these major submission fields and the overall quality of a payer’s submission. The table below shows how a medical claim file may be evaluated to receive a score out of 5.
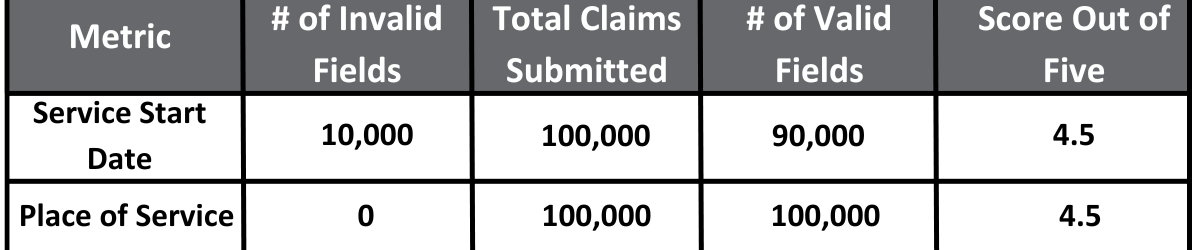
CIVHC is also able to combine these results into a single composite score on a scale of 0 (lowest) to 100% (highest possible), representing the total health of data submitted to the CO APCD. This assessment is completed every other month in conjunction with the bi-monthly data warehouse refreshes and is also made available to individual submitters by CIVHC.
Analysts perform updates to the SQI annually to add additional checks and metrics that enhance visibility into the quality of the CO APCD. In Fiscal Year 2024, the Data Quality team introduced new fields to score collection of demographic data, such as race, ethnicity, and language. The team plans to add new fields each year to align collection fields with the latest updates made to the Data Submission Guide.
CIVHC is currently developing a system to be introduced in a future update to allow payers to receive their scores, creating the opportunity to provide each submitter direct, customized feedback and work with them individually to uplift the quality and completeness of data in the CO APCD.
The SQI score for each data warehouse refresh can be found in the Data Warehouse Refresh Flier, which records the paid through dates and SQI score for each bi-monthly data warehouse refresh. The current flier can be found on CIVHC’s Data Quality and Analytics page.
*Certain claim types, like Medicare Fee-For-Service, have different submission cycles and have a longer “lag time” between paid-through date and availability in the CO APCD. With commercial and Medicaid submissions, the CO APCD represents data with claims paid-through two months prior to processing following each refresh. For example, a data warehouse refresh in May reflects claims paid through February.
Click here to see current paid through dates and a schedule of upcoming warehouse refreshes.