The latest version of the interactive CO APCD Insights Dashboard shows that the Colorado All Payer Claims Database (CO APCD), one of the most robust APCDs in the nation, now contains over one billion claims. In addition to claims volume, the Insights Dashboard can help users understand how the CO APCD has changed over time by exploring health insurance payer, type of claim/coverage (medical, dental or pharmacy), percent covered lives across counties and more. Due to the comprehensive picture of health care in Colorado that the CO APCD provides, it is being used locally and nationally to improve health and health equity, lower health care costs, and improve the quality of care
Since inception in 2012, the CO APCD has grown in depth and breadth. It contains over 1 billion claims from 40 commercial health insurance plans, Medicare Advantage, Medicare Fee-for-Service (FFS), and Medicaid. The CO APCD represents over 5.5 million lives and encompasses 72% of the medically insured, and 67% of the total population of Colorado.
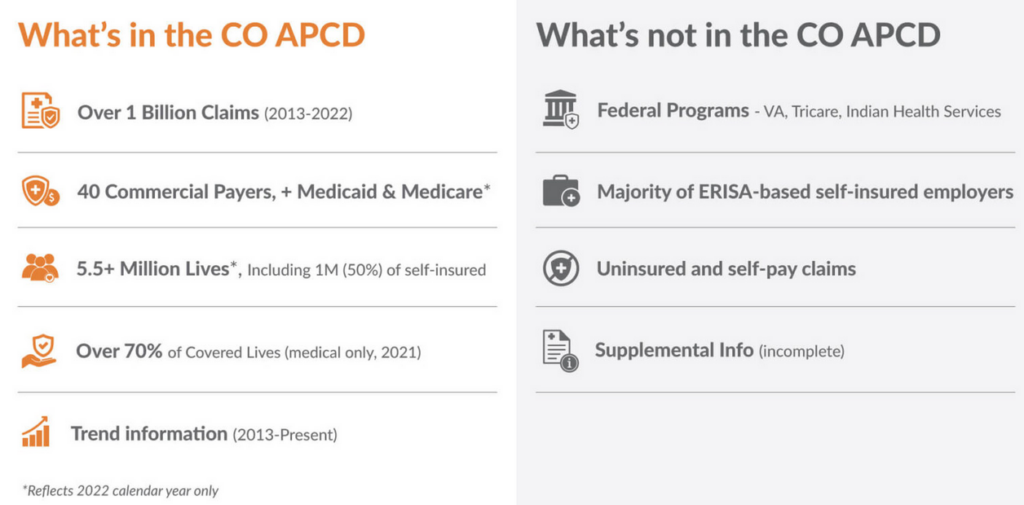
The CO APCD does not contain claims for people covered by Federal health insurance programs such as the Veterans Administration, TRICARE, Federal Employees Health Benefits, or Indian Health Services, and does not include information for uninsured Coloradans. In 2015, the Supreme Court ruled that states are unable to mandate ERISA-based self-insured employers to submit data to APCDs. However, these employers can choose to submit on a voluntary basis. CIVHC estimates that the CO APCD contains 50% of the self-insured employer covered lives, the majority of which are non-ERISA self-insured employers.
Trends in use of behavioral health services are also available in the dashboard and show that the number of visits related to behavioral health continue to increase for Coloradans covered by commercial insurance and Medicaid. The dashboard indicates that between 2013 and 2022, across all payers, over 3.2 million Coloradans accessed one or more behavioral health-related services.
It is important to note that CIVHC collects claims from commercial payers and Medicaid on a monthly basis and updates the entire data warehouse every other month. While the Insights Dashboard reflects claims through calendar year 2022, the data available through CIVHC’s secure data request process is more current and reflects claims paid three months prior (for example, the June 2023 refresh contains claims paid through the end of April 2023).
More information about CIVHC’s role as steward of the CO APCD, how the data is collected, and how it is being used is available in the 2022 CO APCD Annual Report. CIVHC is proud to support Coloradans helping Coloradans and Change Agents across the nation by making CO APCD data available to working to lower costs, improve care, and make us all healthier.
Please visit our website to learn more about public and non-public data and analyses that can be gleaned from the CO APCD, or contact us at info@civhc.org for more information.