The Colorado All Payer Claims Database (CO APCD) contains over 1.3 billion claims, with more added every month. These claims are submitted by commercial health insurance plans, including Medicare Advantage, voluntarily submitted Employee Retirement Income Security Act (ERISA) and mandated non-ERISA self-insured employer plans, Medicaid, and Medicare Fee-for-Service (FFS). The CO APCD does not contain claims for people covered by Federal health insurance programs such as the Veterans Administration, TRICARE federal employees, or Indian Health Services, and does not include information for uninsured Coloradans.
The CO APCD holds information for over 70% of insured individuals in Colorado with medical coverage, representing over 5.6 million lives in total across all coverage types (medical, dental and pharmacy). As of this post, 33 commercial payers submitted claims in 2025 along with Medicaid and Medicare FFS.
This is the middle installment of a series focusing on CO APCD data submitted by payer line of business – commercial health plans, Medicaid, and Medicare (FFS and Advantage). The data in each line of business has different nuances that are helpful to be aware of when using the CO APCD.
Managing Medicaid in Colorado
The Department of Health Care Policy and Financing (HCPF) administers Health First Colorado (Colorado’s Medicaid program). Health First Colorado provides physical, dental, and mental health benefits to qualifying adults and pregnant women as well as children under 18 through the Child Health Plan Plus (CHP+). To help facilitate these benefits, HCPF divided the state into regions and designated organizations in each called Regional Accountable Entities (RAEs) to help patients navigate the system and access services. Additionally, some members opt to enroll in Managed Care Organizations (MCOs), which may offer enhanced care coordination, additional services, or a more integrated provider network compared to the standard RAE model. HCPF and the health plans who act as MCOs or RAEs submit claims for Medicaid members to the CO APCD each month.
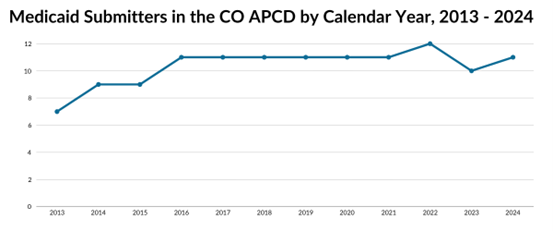
When considering Medicaid submissions, CIVHC employs the same methodology as when calculating lines of business within commercial “payer families.” The MCOs and RAEs are considered submitters to the CO APCD while Medicaid is the overarching payer.
Medicaid Members in the CO APCD
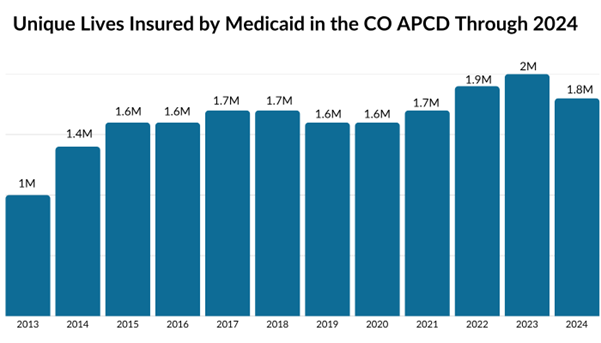
Approximately 26% of Coloradans receive health care services through Medicaid compared to 23% for people with commercial insurance. In 2024, 1.8 million unique individuals were covered under Medicaid programs, and from 2013-2024, the CO APCD includes nearly 5.1 million unique Medicaid members. The CO APCD collects 100% of the claims from Medicaid members in Colorado, making it one of the most complete payer data sets in the database. The robust nature of the Medicaid data set makes it a relatively straightforward asset to use and analyze, unlike commercial data which is subject to self-insured employer submission restrictions or Medicare Fee-For-Service, which can only be used in specific situations.
There are some crucial nuances in how Medicaid pays providers and what is included in the claims submissions that are important to note. Medicaid pays hospitals supplemental payments outside of the typical fee-for-service claim payment, and CIVHC receives a separate annual file indicating additional inpatient payments. These additional payments are included in some of our public reports, such as the per-person-per-year cost information in the Community Dashboard, but may not always be reflected in other reports. In addition, Medicaid pays for services that are not covered by commercial payers (e.g., long-term care services and nursing facilities), so it is important to keep this in mind when comparing Medicaid inpatient costs with inpatient costs from other payer types in our public reports.
For more information about Medicaid claims or other payers submitting to the CO APCD, please visit our CO APCD Insights Dashboard, or contact us at info@civhc.org.