Previous queries have outlined that the CO APCD contains medical, dental, vision, and pharmacy claims for the majority of insured individuals in Colorado, roughly 74 percent of covered lives in the state. However, numerous other behind-the-scenes factors provide insight into how an individual interacts with the health care system.
One of the ways the CO APCD is unique among APCDs is the collection and utilization of data around these less explored components within the health care system that impact cost and quality. Incorporating this additional information allows CIVHC to create a fuller picture of how Colorado’s health care system is functioning. The next few queries in the series will explore these additional types of data elements collected in the CO APCD. This query will address prescription drug rebates, and a future query will address Alternative Payment Models and other non-claims data collected in the CO APCD.
Collecting Prescription Drug Data
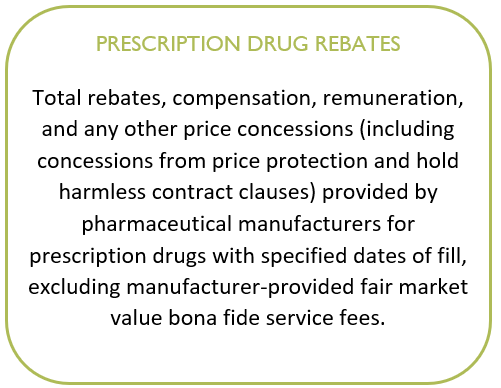
Prescription drugs represent one of the nation’s most significant drivers of rising health care costs. But the system through which they move is historically opaque, and until recently, not much was known about dollars associated with drug rebates collected by commercial payers in Colorado.
To address this issue, and as a part of state efforts to constrain health care costs, CIVHC began collecting drug rebate information in 2018 to start understanding how dollars are exchanged in the system and whether any savings from rebates are being passed along to consumers or employers.
CIVHC used this data to release the first CO APCD interactive report analyzing prescription drug spending and rebates in 2021, and continues to refresh the report annually. The newest update to the report, incorporating data from 2019-2023, was released in April.
The Prescription Drug Affordability Board
Recent versions of the Data Submission Guide (DSG) included substantial updates to submission requirements of prescription drug data to support state-led initiatives to reduce costs.
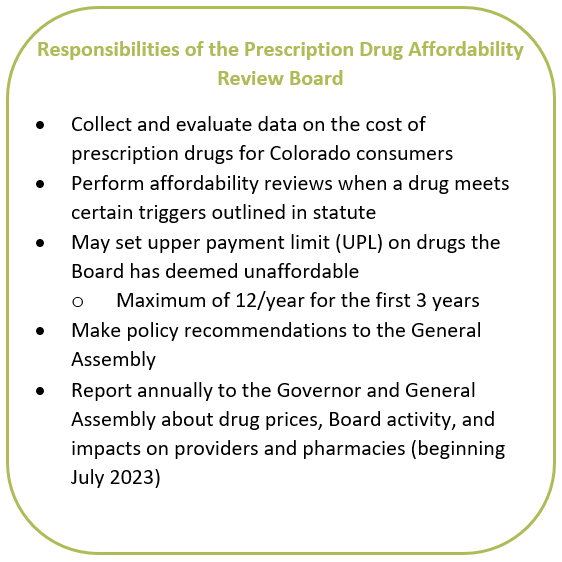
Established under Senate Bill 21-175, the Prescription Drug Affordability Board (PDAB) is housed within the Colorado Division of Insurance (DOI) and is tasked with the responsibility of reviewing the costs associated with prescription drugs, evaluating their affordability, and making recommendations on ways to address costs and potentially setting upper payment caps for certain drugs.
The bill named the CO APCD as a primary source of information to support the PDAB, and while it already contained a good deal of pharmacy claim information, the legislation required introduction of new annual files to support the PDAB’s work:
- Data elements allowing the PDAB to see the drugs accounting for the highest costs in Colorado
- Data regarding value-based pharmaceutical contracts (VBPC) to understand how prescription reimbursements are structured
Unlike claims data, which is collected from payers monthly, pharmacy data files are reported by payers annually and collected each September according to the rules laid out in the DSG. The first prescription drug annual files were reported to the DOI in 2023, and last year the PDAB placed its first prescription drug price cap.
CIVHC continues to collaborate closely with payers to further clarify and refine the submission process to support this state-led work. Files will continue to be collected annually, and per the rule change requirements for this information, is reported directly to the DOI and is not available in non-public reports.
If you have questions or want more information on prescription drug data collected in the CO APCD, you can reach us at info@civhc.org.