Collecting reliable and complete patient demographic data, especially race and ethnicity information, is a challenge most health data organizations, including other state All Payer Claims Databases (APCDs), have grappled with for years. However, all agree that this data is essential to help communities understand drivers, inform solutions and assess progress towards achieving health equity.
As administrator of the CO APCD, CIVHC has been working with payers for years to improve collection and completeness of demographic information including race and ethnicity data. While CIVHC is not exempt from the significant challenges payers themselves face with collecting accurate and complete race and ethnicity data, these fields in the CO APCD have improved over time, especially for commercial insurance payers.
Through consistent, conscientious effort and collaboration with state partners and payers, demographic data in the CO APCD is continually becoming more actionable and insightful, especially when paired with external socioeconomic data.
Race and Ethnicity Data in the CO APCD
Submitting race and ethnicity data became a requirement for payers in late 2019 when a Data Submission Guide update mandated submission of one race and one ethnicity field. CIVHC modeled the data requirements on the guidelines of the U.S. Office of Management and Budget (OMB), which include an indicator for Latino/Non-Latino and five race fields: American Indian or Alaska Native, Asian, Black or African American, Native Hawaiian or Other Pacific Islander, or White. CIVHC also enables payers to select race as “other” or “unknown.”
The OMB updated its race/ethnicity standards in March of 2024, most notably adding a “Middle Eastern and North African” race category and requiring more detailed collection of race/ethnicity data. CIVHC is working with payers in Colorado, including the Department of Health Care Policy and Financing (HCPF), to determine when to add the new standard data elements to the DSG so payers can begin utilizing the additional fields.
Medicare FFS and Medicaid have the most complete race and ethnicity data, and Medicare Advantage data has improved significantly over time.
Commercial payer race and ethnicity data is improving, but challenges remain. The biggest barrier for commercial payers is that they do not consistently collect this information from their members, or their members may be reluctant to report this information. This lack of available data for commercial payers results in large percentages of “unknown” entries compared to Medicare and Medicaid. However, for all payers, race and ethnicity submission completeness has been slowly improving, making the data more and more valuable for understanding the impact of race and ethnicity on health disparities.
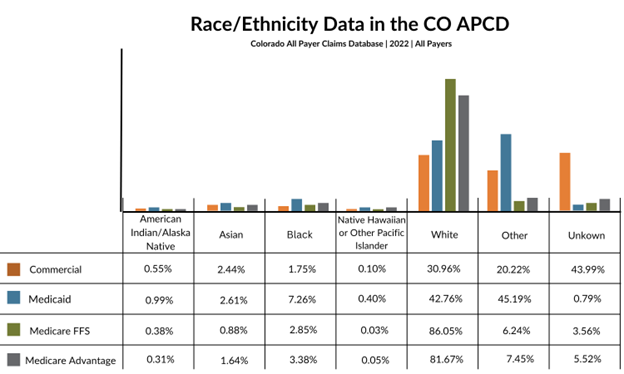
Users can further investigate race and ethnicity data in the CO APCD by payer type and year on CIVHC’s Insights Dashboard page. Starting in July 2025, race and ethnicity data will be included in the demographics tab of the Insights Dashboard along with age and sex information.
Age, Sex and Geographic Demographic Data Collected in the CO APCD
In addition to race and ethnicity data at the person level, the CO APCD has always captured information related to age, sex (male or female), and geographic location based on member residence.
In more recent years, CIVHC added two additional data fields to inform health equity work:
- In 2022, under DSG 13, CIVHC added a new field to capture members’ preferred language.
- In 2020, under DSG 12, a “non-binary” field was added as an option for sex.
Similar to race and ethnicity data, language preference and non-binary sex indicators aren’t always consistently collected by payers, and therefore not available to report to the CO APCD. It is also difficult for CIVHC to validate the completeness of these two fields as there is no external data source for validation. For more information on completeness or volume of claims with a language preference or non-binary indicator, please contact us at ColoradoAPCD@civhc.org.
Next Steps and Additional Data Sources
CIVHC plans to continue to work with payers to improve race, ethnicity, language preference and non-binary sex reporting and will continue to track progress in data submissions. In addition, CIVHC has also taken steps to understand social needs or Z-Codes in the database, and has created infrastructure that allows alignment of the CO APCD data with social demographic information. By geocoding (or assigning latitude and longitude coordinates) people and providers in the CO APCD (the topic of an upcoming Query), external census-tract level social demographic information such as income level and education can be overlaid with information in the CO APCD to conduct additional analyses to understand health inequities.
If you have additional questions about race and ethnicity or other demographic data in the CO APCD, visit our website at www.civhc.org or contact us at info@civhc.org.