As administrator, CIVHC is required by statute not only to maintain the database, but to continually improve the quality and utility of the Colorado All Payer Claims Database (CO APCD). One of the most important ways CIVHC fulfills this part of the charge is through updating the CO APCD Rule and Data Submission Guide (DSG) each year . This is done in collaboration with the Department of Health Care Policy and Financing (HCPF), Division of Insurance (DOI), and health insurance payers across the state.
CIVHC follows the HCPF Executive Rule Change Process to propose new data submission requirements and updates through which new data elements are added, clarified, or eliminated as needed and the language of the CO APCD Rule (Colorado Regulation 1.200) is updated in accordance. Each update CIVHC proposes is to ensure the data is as robust, comprehensive, accurate and usable as possible to provide the most benefit to Colorado. Generally, these updates include:
- standardization or clarification of elements already being collected,
- addition of new elements that will either further align CO APCD data submissions with the Common Data Layout (CDL) being used by APCDs throughout the nation, or
- increase its ability to support and inform efforts to improve health care for Coloradans.
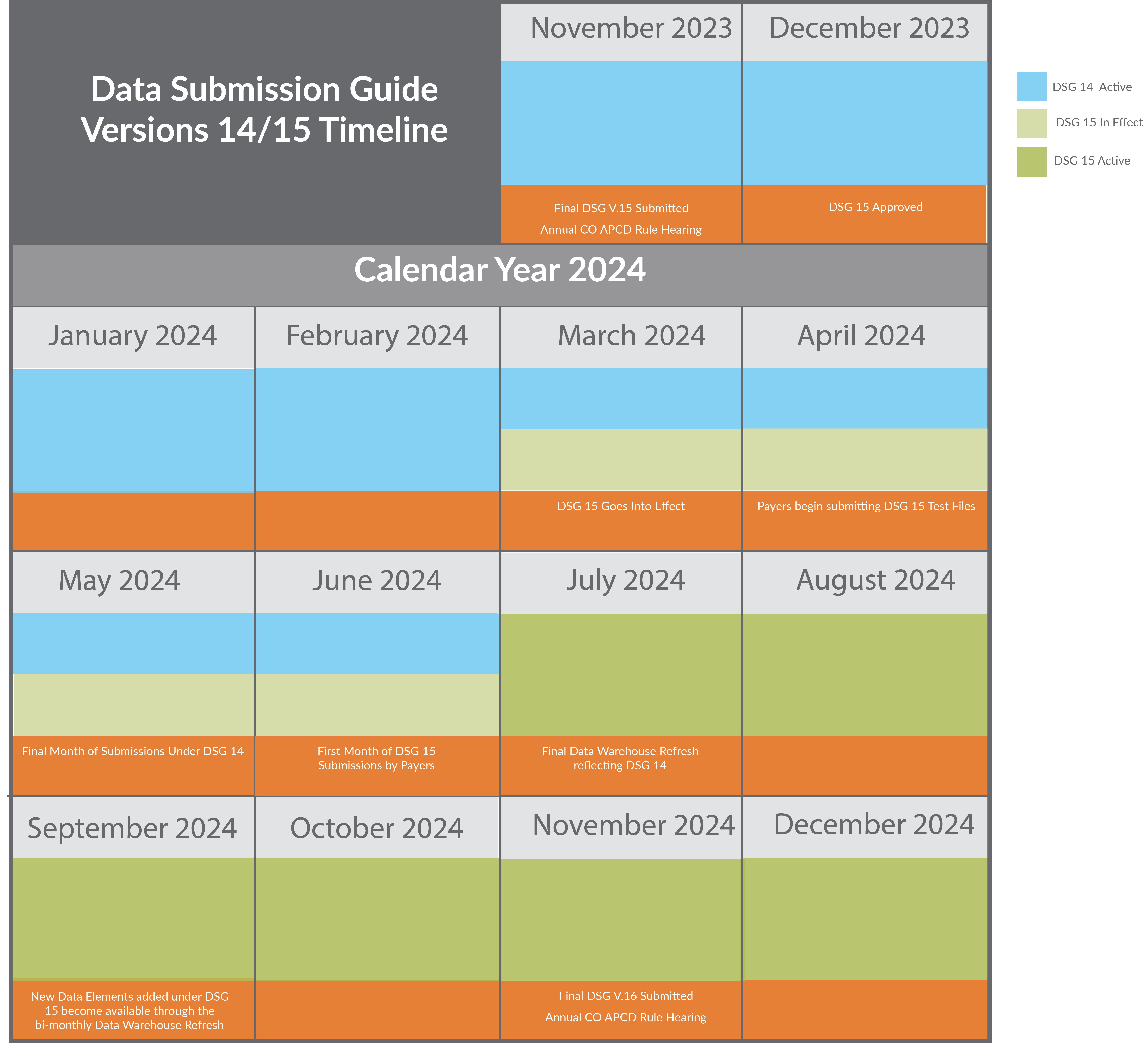
Each DSG update and Rule Change cycle takes place over a year. The CIVHC team started looking toward changes to DSG 15 in early 2023, immediately after approval of changes proposed for DSG 14. Throughout the summer and fall, CIVHC hosted several calls with payers to describe the proposed changes, answer questions, and receive feedback. After multiple drafts, payer feedback calls, comment periods, and virtual public review meetings, CIVHC presented the final proposed changes to HCPF and received approval in November 2023.
DSG 15 and the revised CO APCD Rule will take effect on March 1, 2024. DSG 14 will remain active until June 2024, with payers having a 120-day grace period from the effective date to prepare their systems and submit test files before formal collection of files later this year. Payers’ first submissions of files under DSG 15 will be required in July 2024.
CO APCD Rule
Updates to the 2024 CO APCD rule included two substantial new reporting requirements introduced in DSG 2015:
- Vision Claims Data – Under DSG 15, payers will begin required submission of vision claims in addition to the submission of medical, dental, and pharmacy claims already collected in the CO APCD.
- Wholly Denied Claims – Payers will now also be required to submit wholly denied claims across all claim types. While payers were previously required to submit partially-denied claims, the addition of wholly denied claims reporting will build a more comprehensive picture of health care landscape in Colorado.
Additional updates to the CO APCD Rule were minimal and involved updating dates and titles to fall into alignment with DSG 15.
DSG 15
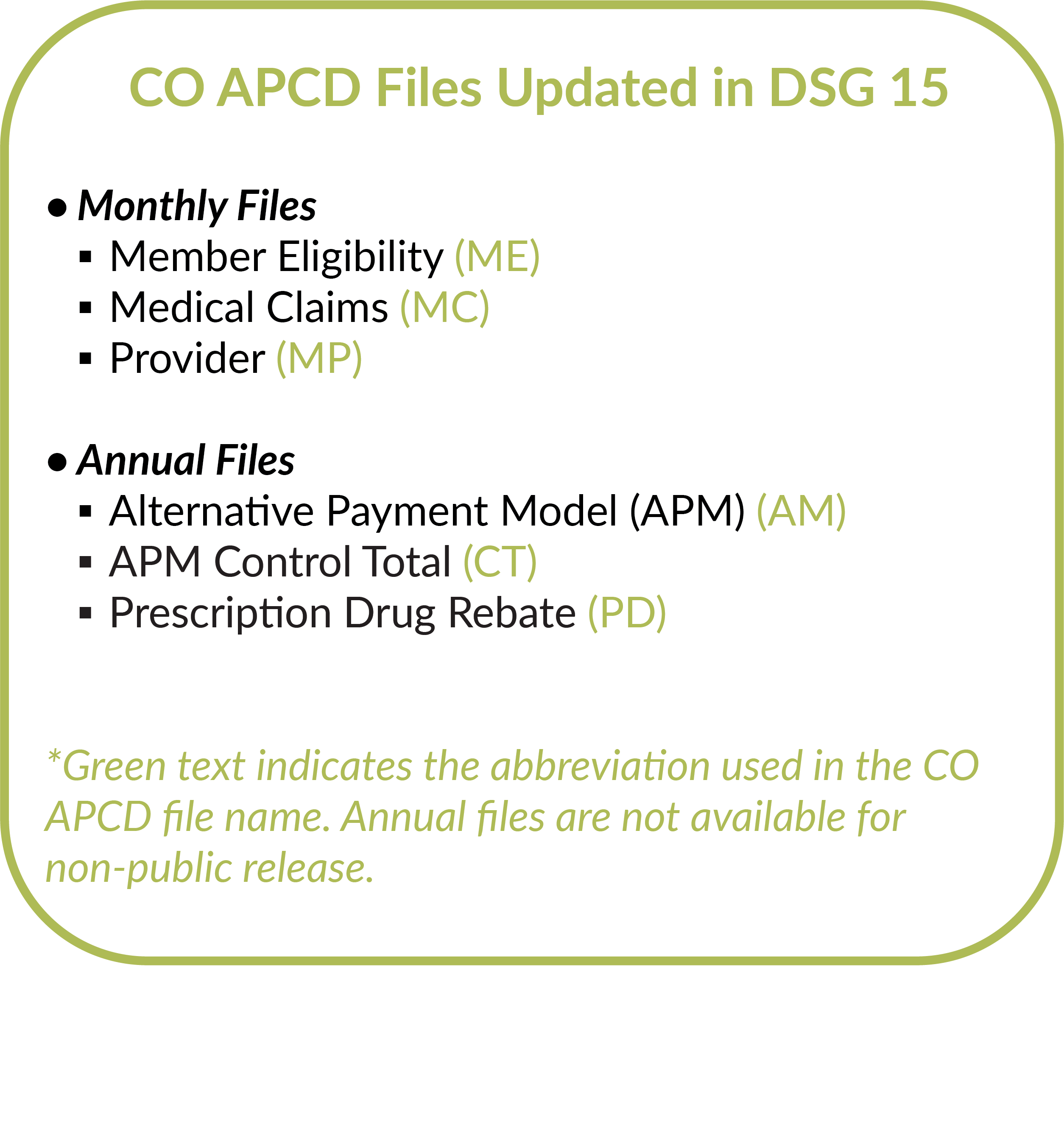
DSG 15 introduces several notable updates to file collection, including multiple new data element fields in accordance with the newly-introduced vision and wholly denied claims reporting requirements. CIVHC collaborated with payers throughout the last year as they worked to integrate these reporting enhancements into their systems, and the process is still ongoing to ensure timely, accurate submission of these files.
Guidance for payers and data element reporting requirement updates were included across file types to integrate vision and denied claims collection. In addition, further notable updates to DSG 15 to improve submission quality are outlined below.
Monthly Files: Membership Eligibility & Provider Updates
The most significant additions to the Membership Eligibility files Are:
- Addition of a Vision Coverage Field – An indicator to identify members with vision coverage.
- Updates to the Regional Accountability Entity (RAE) Indicator – A RAE is an organization under Colorado’s Medicaid program responsible for coordinating care, ensuring access, and identifying strategies to improve care. An indicator identifying these organizations is important to enable analysis of Colorado’s Medicaid program, and was introduced in DSG 14. DSG 15 includes updates to guidance language and reporting requirements around this indicator.
An additional noteworthy addition is made to Provider files:
- Addition of a Provider Health System Affiliation field – This field captures a provider’s employment affiliation with a health system to understand specific provider relationships with health systems. We will review the data submitted in this field to determine if additional guidance is needed. This field will likely continue to undergo refinements as CIVHC receives feedback from submitters.
Annual Files Updates
The most significant additions to the annual files are the inclusion of new fields across all file types to reflect the collection of vision and denied claims data.
As payers work to prepare for changes under DSG 15, CIVHC is already working to develop DSG 16 in anticipation of what elements, insights, and data collection enhancements will keep the CO APCD at the forefront of claims analysis.
If you have questions regarding DSG 15 or would like more information on completeness and availability of data, please contact info@civhc.org.