Project Name: Provider Payment Tool

Project Purpose: The Provider Payment Tool is required by SB 22-068, and displays provider reimbursements for different services as well increases price transparency in Colorado.
Analyst: Tim Ginader, MS, Senior Health Care Analyst, Team Lead
1.) What were your first steps when beginning this analysis?
This project is designed to display the range of costs for health care procedures throughout the state. The first step was to develop a methodology to determine how to define the procedures and accurately calculate their rates.
2.) Were there specific considerations you needed to consider based on the data?
One of the biggest considerations was how to handle anesthesia claims as they are billed much differently from other claims. We ended up creating a separate dashboard for anesthesia claims where users can input procedure-specific-specifications to see rates.
3.) What challenges did you encounter while performing the analysis? How did you overcome them?
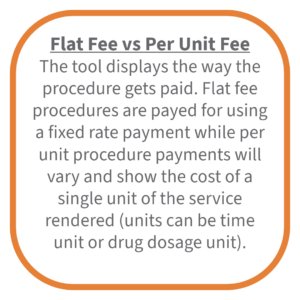
This project contained many challenges including how to account for flat-fee procedures vs per-rate procedures, how to deal with in-network vs out-of-network claims, and how to calculate amounts for specialty procedures relating to COVID or medical transportation. The team discussed all of these challenges and developed a methodology to account for each of them.
4.) Without delving into results, did anything surprise you about this analysis or the process of executing it?
On first glance, calculating average and percentile costs for each procedure seemed pretty straightforward. I was surprised at how un-straightforward it ended up being.
5.) What did you learn while performing this analysis?
I learned that having an initial analytic plan and methodology to begin a project like this is crucial. These can always be changed and adjusted as the project progresses, but having a baseline is key.