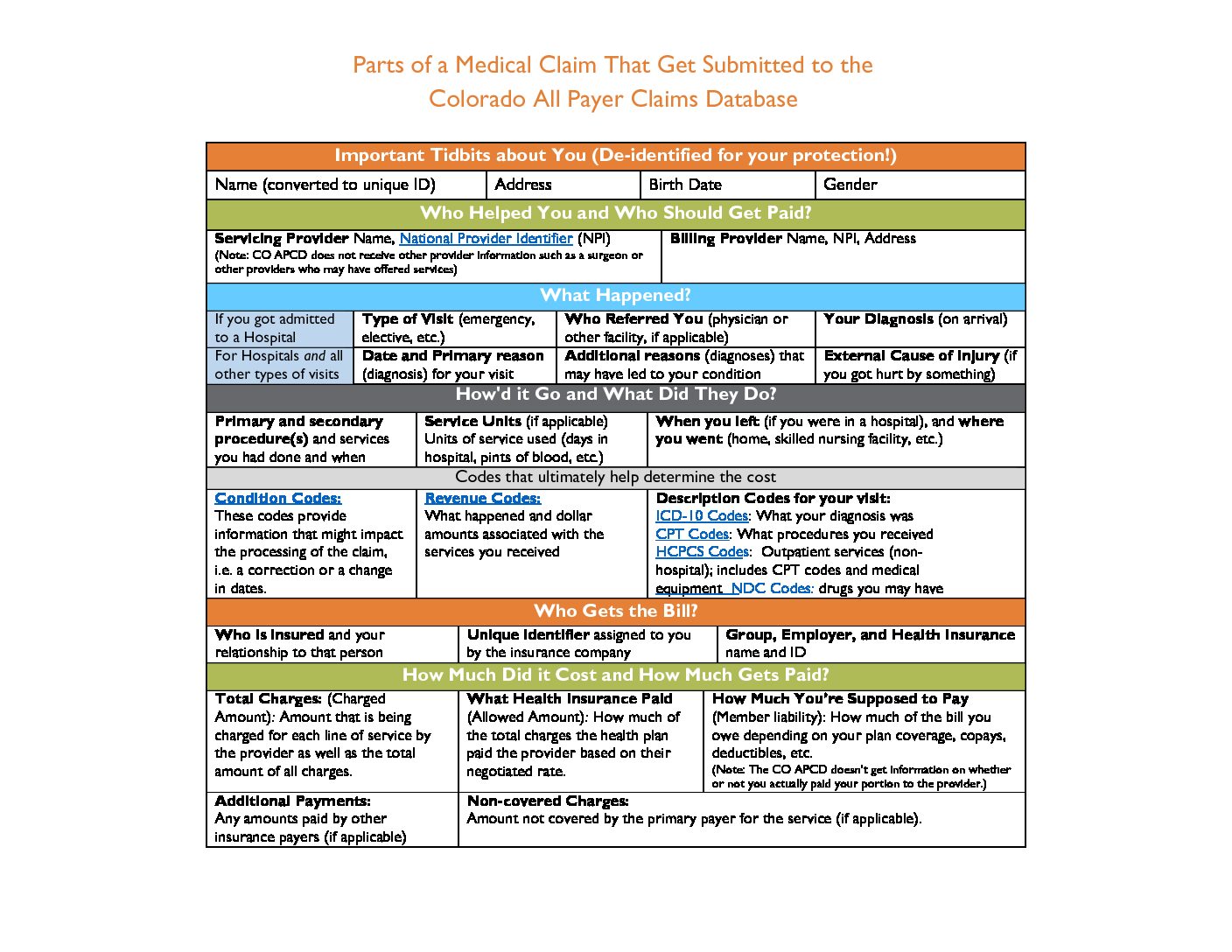
This is the first in a series of blogs about what exactly is in the Colorado All Payer Claims Database (CO APCD). Today we’re looking at one of the most fundamental claims we receive – the medical claim. Medical claims include basic information about why you went to the doctor or hospital, who you visited, and what happened while you were there – all information which forms the basis for the facility (hospital or provider group) part of the cost of the visit.
Sometimes really cool things are made up of really boring parts; take the Internet for example. When we log on to Facebook, we’re seeing a finished page that has pictures and text and lots of exciting ways to interact with the content. But, on the backside, Facebook is nothing more than a bunch of computer code:

The CO APCD is pretty similar. To file a claim, providers fill out a form that has a bunch of tiny boxes and submit it to the insurance company. After processing by the payer, the claim ends up in the CO APCD, and is even more complicated to look at than the form (how is that even possible?).

However, in the same way that each line of computer code gibberish translates to something cool, each of the boxes on an insurance claim contains information that can be used to do something pretty awesome.
Now, different types of facilities and providers fill out different versions of these forms so rather than explore a bunch of really boring forms, we’re going to use a general example to show what kind of information is provided in a typical medical claim. Additionally, we’re only focusing on what is collected by the CO APCD and not delving into any privacy or security concerns – all that stuff is coming, don’t worry, we want to take this step by step and not drop too much info on y’all all at once.