![]() What are bundled payments, and how do they help providers reduce waste and deliver better care?
What are bundled payments, and how do they help providers reduce waste and deliver better care?
In the past decade, the health care system has started shifting away from volume-based payments (payments per visit regardless of the outcome), to a value-based payment (payments tied to quality and/or outcomes) approach. This was a move by health insurance payers to encourage providers to minimize waste and improve overall care. 
The journey to a successful value-based health system is complex and even experts are unsure how long it will take for these programs to be successful. However, in the long run, new payment models have the potential to improve care coordination, increase quality of care, and allow for a greater understanding of cost drivers so providers can target interventions and focus on improving overall health.
So, how do we start?
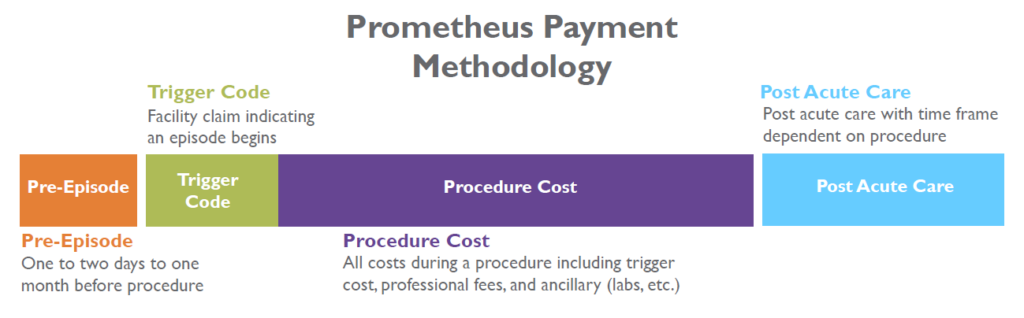
Bundled payments, also known as episode-based payments, are one example of value-based payments that are a relatively easy place to start, and are beginning to be implemented more widely. Bundled payments were created by payers as a way to incentivize care coordination and excellent outcomes by providing one payment for all care before, during, and after a service. In other words, instead of paying each provider and facility separate amounts for their involvement in a knee replacement, for example, the episode payment is pre-determined and includes the consultation, the procedure, and follow-up care like therapy and rehab.
This type of payment structure encourages health care professionals to understand not only their own costs, but also to work with other providers to ensure patients receive excellent care throughout the episode, and identify cost saving and quality improvement opportunities. In the past decade, providers and payers have voluntarily implemented bundled payment arrangements, and more recently, The Centers for Medicare and Medicaid Services (CMS) has started implementing bundled payments for procedures such hip and knee replacements and cardiac care.
Think of a bundled payment as a perfectly crafted sandwich that has been pre-defined to be worth $10.00 to the payer (health insurance company) based off of what other restaurants charge. Let’s say the payment for the meat is $5.00, the bread is $2.50 and any “extras” or toppings are $2.50. In this analogy, the procedure being done, or the “main event” is the meat in the sandwich. The meat portion of any sandwich tends to vary based on the restaurant’s food distributor, the quality of the meat, and the quantity that the restaurant decides to include, but in order to make a profit, the meat needs to be both affordable and excellent so customers will buy it and be satisfied.
The pre-care and post-care are the bread holding the sandwich together, and without the bread, a sandwich wouldn’t be a sandwich. Pre- and post-procedure care is key in creating an excellent sandwich (or patient outcome) and also must take into consideration how to provide the care for $2.50 or less.
The additional toppings in this sandwich analogy are some of the post-acute and pharmacy services, with many being necessary, but some being optional or unaffordable to the patient. For example, many people believe that a sandwich needs lettuce and tomato to be complete, while some believe cheese and mustard is where it’s at. There is an ideal amount of “add-ons” for each sandwich, before the sandwich becomes large, unmanageable, or there are so many items included that some aren’t even enjoyed.
In the same way that restaurants have different pricing, facilities and providers do as well, and tools like www.comedprice.org can show consumers how costs can vary. In a restaurant setting, a higher price doesn’t necessarily mean that the meat is better or worse quality. The same is true for facilities, which is why understanding quality in a bundled payment becomes as important as cost. It is the health care provider’s responsibility to help each patient understand what is included in a “perfect sandwich,” while still paying attention to the idea that resources are finite, and not every sandwich can have all the toppings. Bundled payments help providers identify these “extras” by making them look at the care necessary to have the most ideal outcome and pre- and post-care with the least amount of waste.
And what if your sandwich was not made to your specifications and somewhere along the way you didn’t get the bread or quality meat you anticipated? The restaurant would have to make you another one at no cost. Same goes for bundled payments for procedures. If you experienced an avoidable complication because something in the process broke down, the providers involved don’t get paid to remedy the problem like they used to. Therefore they have an incentive to do it right the first time and make sure you get the results you deserve.
So let’s recap:
- Bread = Pre- and Post-Episode or Procedure Care
- Crucial elements on each side of the “main event.”
- Meat = Procedure
- The “main event,” which can be obtained at a varying cost or quality from many facilities.
- Toppings = Additional pharmacy and post-acute services
- Sometimes necessary, and many times optional. Should be limited to those things that improve patient outcomes and experience. Greatly vary based on provider choice.
Overall, it’s been shown that bundled payments can slash costs for complex episodes of care such as oncology care. By incentivizing providers through reimbursement rates, it creates a need for greater attention to detail and a better understanding of how patients are being referred for, and in turn using health care services. The hope is that as programs continue to be created and implemented by CMS and the commercial market that the American health care system will continue to move one step closer toward the vision of the Triple Aim – better health, better care, lower costs.